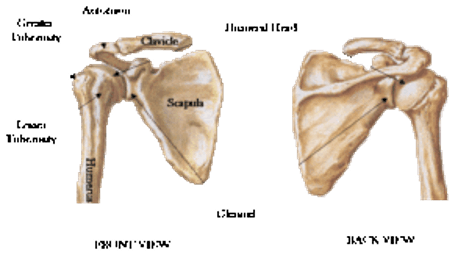
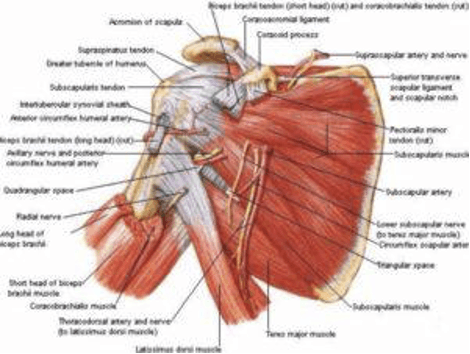
Shoulder Anatomy
To understand why your shoulders hurt, it helps to know a little bit about your shoulders’ anatomy. Shoulder joints give you a wide range of motion, but this can also make them susceptible to injury. Your shoulder is a ball-and-socket joint, with the ball part located on the humerus bone and the socket part on the scapula bone. Each shoulder also has a collarbone called a clavicle. Surrounding and supporting your shoulder bones are several muscles and tendons called the rotator cuff.
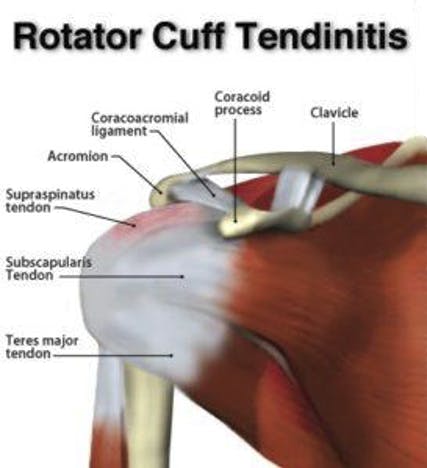
1. Rotator Cuff Tendonitis
Because of its important job and the stress placed on it, your rotator cuff is very susceptible to injury. One common type of rotator cuff injury is rotator cuff tendonitis. Tendonitis simply means inflammation and swelling of tendons–the tissue that connects muscle to bone. There are several reasons rotator cuff tendons may become inflamed, including repetitive movements, sports injuries, aging, and poor posture. Many people suffer from shoulder tendonitis because of movements required by their jobs. Symptoms include swelling and pain, particularly in the front of the shoulder. Fortunately, physical therapy is a very effective treatment for rotator cuff tendonitis.
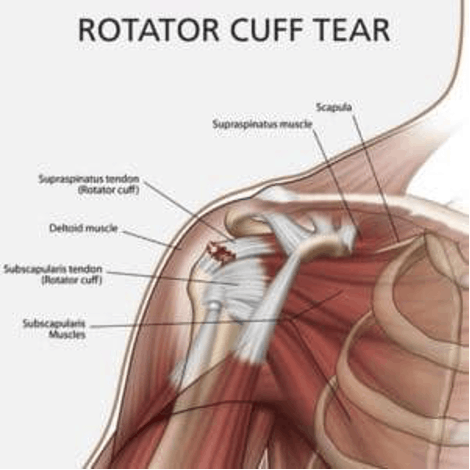
2. Rotator Cuff Tear
Another type of rotator cuff injury is a rotator cuff tear. This tear is often caused by an injury or aging. Symptoms of rotator cuff tear include weakness and pain in the shoulder. If the tear was caused by a traumatic injury, this pain can sometimes be severe. In most cases, physical therapy and other conservative approaches can help heal a rotator cuff tear. In some severe cases, surgery may be necessary.
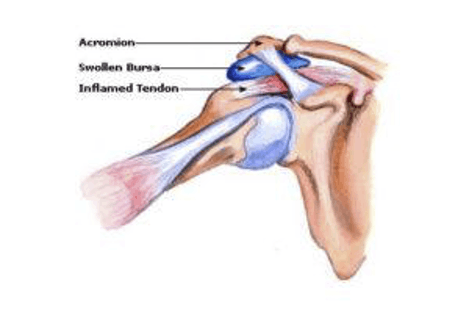
3. Bursitis
A bursae is a fluid-filled sac that cushions the areas around many types of joints. Bursitis occurs when bursae become inflamed. According to the Mayo Clinic, bursitis normally occurs because of repetitive movements, or because of pressure put on the bursae for long periods of time. Shoulder bursitis symptoms include achiness in the joint, pain with movement and swelling. Rest, icing, physical therapy, and other conservative treatments usually help to alleviate bursitis pain.
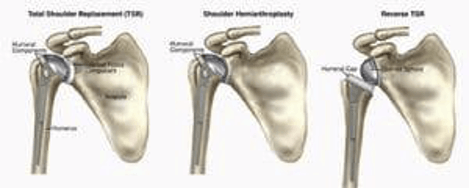
4. Arthritis
Arthritis is joint pain caused by joint inflammation. There are several types of arthritis, the most common of which are osteoarthritis and rheumatoid arthritis. In the United States, arthritis the leading cause of disability, with an estimated 50 million adults suffering from the condition. Arthritis is more common in older adults, females, and those with a family history of the condition. Symptoms of arthritis in the shoulder include pain that gets worse with activity and limited range of motion. Arthritis responds well to physical therapy and exercise.

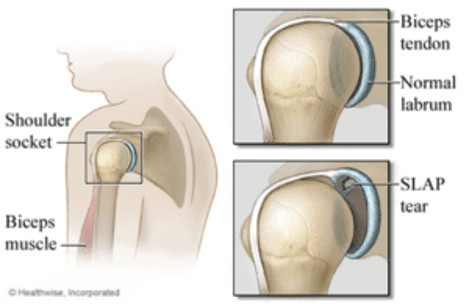
5. Labral Tear
A tissue called a labrum helps to cushion your shoulder socket. This tissue can become torn, causing shoulder pain. Reasons for a labral tear include traumatic and overuse injury. Symptoms may include a popping sensation followed by aching and pain. Your shoulder may feel like it is catching on something when you try to move it.
What Can You Do About Shoulder Pain?
If you’re experiencing shoulder pain that doesn’t go away on its own, you should schedule an appointment with a physical therapist or doctor. All of these common causes of shoulder pain can greatly benefit from an individualized physical therapy plan. Additionally, over-the-counter non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen can help to decrease inflammation.
Conservative approaches to treating shoulder pain are often the most effective. In some severe cases, surgery or injections may become necessary, but these measures should only be taken as a last resort.
A well-trained physical therapist like the shoulder pain experts at Hess Physical Therapy can distinguish between these types of shoulder pain and create a treatment plan for you. For more information or to schedule an appointment, call any of our Hess Physical Therapy locations or refer to our website for further contact info.
Our locations:
- Kennedy: (412)-771-1055
- Crafton: (412)-458-3445
- Allison Park: (412)-487-2787
- Bethel Park: (412) 835-2626
- Atlasburg: (724) 947-9999
Website: www.hesspt.com
Disclaimer: this information is "not medical advice" and is used at the site visitor's own risk.