Introduction: Receiving a diagnosis of osteopenia, a precursor to osteoporosis, can be concerning. Many people wonder if there are natural approaches they can take to improve bone density and reduce the risk of fractures before resorting to prescription medications. In this blog post, we will explore various factors that influence bone health and provide actionable steps to enhance bone density without relying solely on medications.
Factors Affecting Bone Density:
- Weight and Body Mass Index (BMI): Contrary to common belief, having a slightly higher weight, preferably within the normal BMI range, can be protective for bone density. Additional weight places stress on the bones, stimulating the process of bone remodeling, which can lead to increased bone strength.
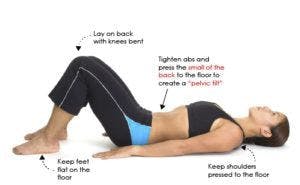
- Weight-Bearing Exercise: Engaging in weight-bearing exercises such as jogging or walking is essential for improving bone density. These activities subject the bones of the spine and hips to the effects of gravity and help promote bone remodeling. Swimming, while beneficial for overall fitness, does not provide the necessary weight-bearing stimulus to enhance bone density.
- Resistance Training: Incorporating weight training exercises into your routine can have a positive impact on bone health. Lifting weights at a sufficient intensity causes micro-tears in muscle fibers, which in turn stimulates the remodeling of bone tissue. By strengthening the muscles attached to the bones, weight training contributes to overall bone strength.
Hormonal Influences:
- Menopause and Hormonal Changes: The onset of menopause leads to a decline in estrogen levels, which results in an increased risk of osteoporosis and osteopenia. Estrogen plays a crucial role in inhibiting bone breakdown by suppressing osteoclast activity. Additionally, progesterone promotes the action of osteoblasts, cells responsible for building bone. The decline in these hormones contributes to bone loss, making post-menopausal women particularly vulnerable.
- Cortisol and Stress: Elevated levels of cortisol, the stress hormone, can cause bone thinning and contribute to osteoporosis. This hormone, released in response to stress, can cause the bone to break down more quickly. Managing stress levels and reducing the use of corticosteroid medications whenever possible are crucial steps in preserving bone density.
- Thyroid Health: Hyperthyroidism, whether due to autoimmune conditions or excessive thyroid replacement, can lead to bone thinning and osteoporosis. Ensuring optimal thyroid function is essential for maintaining healthy bones.
Nutritional Considerations:
- Micronutrients: Supplying the body with the necessary substrates and minerals is vital for improving bone density. Key minerals include magnesium, calcium, and boron. Incorporating these minerals into the diet or using appropriate supplements can support bone health.
- Vitamin D3 and Vitamin K: Vitamin D3 aids in the absorption of calcium, whether from dietary sources or supplements. Vitamin K2 helps direct calcium to the bones, preventing its accumulation in undesirable areas such as the kidneys or blood vessels. Combining adequate vitamin D3 and vitamin K2 intake ensures calcium is properly utilized by the bones.
- Dietary Choices: An alkaline diet can help maintain optimal bone health. Acidic foods, such as sugars, breads, and pastas, can contribute to calcium depletion from bones. In contrast, alkaline foods, primarily vegetables, promote a more favorable pH balance and support bone density. A well-rounded diet should consist of approximately 75% alkaline foods, including vegetables, lean meats, fish, and complex carbohydrates.
Conclusion: Taking control of bone health and preventing osteopenia and osteoporosis involves a
multifaceted approach. By adopting lifestyle choices that promote weight maintenance, engaging in weight-bearing exercises, incorporating resistance training, optimizing nutrition and addressing hormonal imbalances, we have many tools to help improve bone health.
The Hormone Center is an integrative medical practice specializing in thyroid treatment, adrenal gland support and Bioidentical Hormone Replacement Therapy in Carnegie, Pennsylvania. If you would like more information on balancing hormones for optimal health, please visit Bioidentical Hormone Replacement Therapy or call 412-432-7909.
*These statements have not been evaluated by the Food and Drug Administration. These products are not intended to diagnose, treat, cure, or prevent any disease.
Disclaimer: The information provided in this blog post is for educational and informational purposes only and is not intended as medical advice. It should not be used to diagnose or treat any medical condition, nor should it be considered a substitute for professional medical expertise or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read in this blog post.