If you are experiencing pain where the tendons of your forearm attach to the bony bump on the inside of your elbow, you may have a condition known as golfer’s elbow. Even if you don’t play golf, this injury happens to many people over time.
What is golfer’s elbow?
Let’s start by understanding the anatomy of the elbow. The elbow is a joint. It contains three arm bones, the humerus, ulna, and radius. The ends of these bones are covered with cartilage, which allows the joints to absorb shock. The bones are held together by ligaments which form the joint capsule. The joint capsule surrounds and lubricates the joint. There is a ligament on the inside of the elbow and another on the outside of the elbow. These, together with a third ligament holding the radial head against the ulna, keep the elbow stable. The nerves in your arms pass across the elbow. They transmit sensations and tell your muscles to work.
Golfer’s elbow is usually experienced as pain in the medial, or inside, of your elbow. The pain may spread into your forearm and wrist. Your pain may grow worse during forceful arm motions, gripping and lifting.
Why does golfer’s elbow occur?
The method of injury, (MOI) is usually chronic overuse, such as repeatedly twisting the forearm when making throwing or swinging motions. These motions may apply too much force to the area. Sometimes improper technique or equipment used in a sport can contribute to the condition.
How is golfer’s elbow diagnosed?
Diagnosis usually begins with a medical history and physical examination. A doctor may order an X-ray to rule out other possible causes of elbow pain.
Your medical professional may perform a medial epicondylitis test. During this procedure, your doctor or therapist supports the elbow with one hand, extends the elbow, wrist, and fingers and palpates the affected region. If this produces pain or discomfort, the test is considered positive. The doctor may also perform various strength, range of motion and functional mobility tests on your elbow, forearm, and wrist.
What if you are not a golfer?
In addition to golf, many activities can lead to golfer’s elbow. Sports such as racket sports, throwing sports, and weight training can all cause golfer’s elbow. Repetitive tasks like gardening, shoveling, throwing a ball, painting and similar activities all put you at risk for golfer’s elbow. Occupations that require forceful, repetitive movements, such as construction, plumbing, and carpentry, can lead to golfer’s elbow. Other risk factors include smoking and obesity.
Physical therapy
Assessments performed by your physical therapist may be used for differential diagnosis, which helps identify other possible conditions or diseases that could be causing your symptoms. Once your physical therapist has evaluated your condition, he or she will work with you to develop a plan of care. This may include various treatments, such as:
- Ice
- Heat
- Kinesiology taping for your elbow
- Elbow bracing or support sleeves
- Ultrasound
- Electrical stimulation
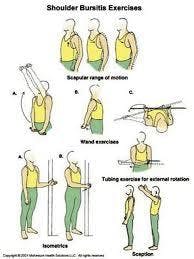
Your physical therapist may prescribe some exercises designed to restore strength to your elbow and wrist, and increase your range of motion. These exercises may include:
- Exercises to increase your elbow joint mobilization
- Exercises to improve the strength and stability of your shoulder area
- Wrist flexor and extensor stretches
- Exercises to strengthen your wrist and elbow
Physical therapy may include Instrument Assisted Soft Tissue Mobilization (IASTM), which may help loosen tight muscles and increase your range of motion. Also, you can learn how to modify your activities to prevent future problems.
What is the difference between golfer’s elbow and tennis elbow?
Both golfer’s elbow and tennis elbow are forms of elbow tendinitis. The difference is simply that golfer’s elbow is caused by damage to tendons on the inside of the elbow, while tennis elbow is a function of tendons on the outside of the elbow.
If you have questions or concerns about possible golfer’s elbow, call Hess Physical Therapy or visit our website for further contact information.
Our locations:
- Kennedy: (412)-771-1055
- Crafton: (412)-458-3445
- Allison Park: (412)-487-2787
- Bethel Park: (412) 835-2626
- Atlasburg: (724) 947-9999
Website: www.hesspt.com
Disclaimer: this information is "not medical advice" and is used at the site visitor's own risk.

 [blog_locations\
[blog_locations\